Arts & Food
Fashion
In today’s fast-paced healthcare environment, digital health records (DHRs), also known as electronic health records (EHRs) or electronic medical records (EMRs), are transforming the way patient information is managed and utilized. By transitioning from traditional paper-based systems to digital formats, healthcare providers are enhancing accuracy, accessibility, and coordination in patient care. This comprehensive guide explores the evolution, benefits, challenges, and future prospects of digital health records.
What Are Digital Health Records?
Digital health records are electronic versions of a patient’s medical history. They include vital information such as diagnoses, treatment plans, medications, and test results. Unlike paper records, digital health records are stored electronically, providing a more streamlined and efficient way to manage patient data.
Evolution of Health Records
1. Paper-Based Records
Before the digital era, patient records were maintained on paper. While this method was functional, it had significant drawbacks, including the risk of loss, damage, and difficulty in sharing information between different healthcare providers.
2. Introduction of Electronic Records
The shift to electronic health records began in the late 20th century. Early EHR systems were primarily used for administrative tasks like billing and scheduling. Over time, these systems evolved to include comprehensive clinical data, enabling better management of patient care.
3. Modern EHR Systems
Today’s EHR systems offer advanced functionalities, including clinical documentation, laboratory results, and patient communication tools. They are designed to enhance care quality, streamline workflows, and improve patient outcomes.
Benefits of Digital Health Records
1. Improved Accuracy and Safety
Digital health records minimize errors associated with handwritten notes. EHR systems incorporate validation checks and alerts to prevent medication errors and other issues, improving patient safety. For example, drug interaction alerts notify healthcare providers of potential adverse reactions, enhancing overall care quality.
2. Enhanced Accessibility
One of the major advantages of digital health records is their accessibility. Authorized healthcare professionals can access a patient’s complete medical history from any location, facilitating coordinated care. This accessibility is crucial in emergencies and supports telemedicine services, allowing for remote consultations and continuous care.
3. Efficient Data Management
EHRs streamline data management by reducing the need for physical storage and minimizing the risk of lost records. Healthcare providers can quickly retrieve, update, and share patient information, which improves efficiency and productivity. Automated features for scheduling, billing, and documentation further enhance operational efficiency.
4. Increased Patient Engagement
Patient portals associated with EHR systems give patients access to their health information. Through these portals, patients can view their records, track their health status, schedule appointments, and communicate with their providers. This increased engagement promotes adherence to treatment plans and better health outcomes.
5. Advanced Data Analytics
EHR systems generate valuable data that can be analyzed to gain insights into patient populations, treatment outcomes, and healthcare trends. This data-driven approach supports evidence-based medicine, allowing healthcare providers to make informed decisions and identify areas for improvement. Population health management and research benefit greatly from the aggregated data in EHR systems.
Challenges of Digital Health Records
1. Data Privacy and Security
The digital nature of health records raises concerns about data privacy and security. Ensuring that patient information is protected from unauthorized access and breaches is critical. Healthcare organizations must implement robust cybersecurity measures, including encryption, access controls, and regular security audits.
2. Interoperability Issues
Interoperability remains a challenge in the realm of digital health records. Different EHR systems may use various formats and standards, making it difficult to share information seamlessly across different platforms. Ongoing efforts aim to develop standardized protocols and improve interoperability.
3. Training and Usability
Effective use of EHR systems requires proper training for healthcare professionals. Issues with poorly designed interfaces and inadequate training can lead to decreased productivity and user frustration. Investing in user-friendly systems and comprehensive training is essential for maximizing the benefits of EHRs.
4. Cost and Implementation
Implementing EHR systems can be costly, particularly for smaller healthcare providers. The expenses associated with software acquisition, hardware, training, and ongoing support can be significant. Balancing these costs with the long-term benefits of digital health records is crucial for healthcare organizations.
5. Legal and Ethical Considerations
Digital health records also raise legal and ethical concerns. Issues related to data ownership, patient consent, and potential misuse of information must be addressed. Establishing clear policies and ethical guidelines is necessary to protect patient rights and ensure compliance with regulations.
The Future of Digital Health Records
1. Artificial Intelligence (AI) Integration
AI is expected to enhance digital health records by providing advanced data analytics, predictive modeling, and decision support. AI algorithms can analyze patient data to identify patterns, predict outcomes, and suggest personalized treatment plans, improving the accuracy and efficiency of care.
2. Blockchain Technology
Blockchain technology offers a secure and transparent method for managing digital health records. By creating an immutable and decentralized ledger, blockchain can enhance data security, streamline data sharing, and ensure the integrity of patient information.
3. Improved Interoperability
Future developments will likely focus on improving interoperability between different EHR systems. The creation of standardized protocols and data exchange frameworks will facilitate seamless information sharing and better care coordination.
4. Patient-Centric Innovations
The next generation of EHR systems will focus on increasing patient engagement and empowerment. Innovations such as personalized health dashboards, real-time monitoring, and integration with wearable devices will provide patients with a more comprehensive view of their health.
Conclusion
Digital health records are revolutionizing healthcare by enhancing accuracy, accessibility, and efficiency in managing patient information. Despite challenges related to data privacy, interoperability, and cost, the benefits of EHR systems are substantial. As technology continues to evolve, digital health records will play a critical role in shaping the future of healthcare, improving patient outcomes, and supporting a more connected and efficient healthcare system.
For more information on how digital health records are transforming healthcare and enhancing patient care, visit WellBeingProTips.com. For more Visit Our Tiktok, Twitter, and Pinterest.
Artificial Intelligence (AI) is rapidly transforming healthcare, offering groundbreaking advancements that significantly enhance patient well-being. From improving diagnostics to personalizing treatment plans, AI is reshaping the healthcare landscape. This article explores how AI is revolutionizing healthcare, including its applications, benefits, challenges, and future potential.
What is AI in Healthcare?
Artificial Intelligence (AI) involves using algorithms and computational models to perform tasks requiring human-like intelligence. In healthcare, AI technologies such as machine learning, natural language processing, and robotics are being used to analyze data, predict outcomes, and assist in decision-making processes.
Key Applications of AI in Healthcare
1. Enhanced Diagnostics
AI is making strides in medical diagnostics by analyzing medical images with high accuracy. AI systems can detect abnormalities in mammograms, CT scans, and MRIs, highlighting potential issues for radiologists to review. Studies show that AI can match or surpass human diagnostic capabilities in areas like cancer detection and diabetic retinopathy.
2. Personalized Treatment Plans
AI enables personalized medicine by analyzing patient data to recommend customized treatment plans. By leveraging genetic information, medical history, and other relevant data, AI can suggest the most effective treatments for individual patients, reducing the risk of adverse effects and improving outcomes.
3. Predictive Analytics for Preventive Care
AI’s predictive analytics can identify potential health issues before they become critical. By analyzing trends and patterns, AI can forecast the likelihood of chronic conditions such as diabetes or heart disease, allowing for early intervention and preventive measures to improve overall patient well-being.
4. Drug Discovery and Development
The drug discovery process is being accelerated by AI. Machine learning algorithms analyze biological data to identify potential drug candidates more quickly. AI also helps design clinical trials by selecting suitable participants and optimizing trial protocols, increasing the likelihood of successful outcomes.
5. Administrative Efficiency
AI improves healthcare efficiency by automating administrative tasks such as scheduling, billing, and medical record management. Natural language processing can streamline the organization of electronic health records (EHRs), reducing the administrative burden on healthcare professionals and allowing them to focus more on patient care.
Benefits of AI in Healthcare
1. Improved Accuracy and Efficiency
AI enhances diagnostic accuracy and operational efficiency by processing large datasets with precision. AI systems analyze medical images and interpret complex data quickly, reducing human error and improving decision-making speed.
2. Cost Reduction
AI contributes to cost reduction in healthcare by optimizing resource use and streamlining operations. Automation of routine tasks and improved diagnostic accuracy lead to fewer unnecessary tests and procedures, while predictive analytics help prevent costly complications.
3. Increased Accessibility
AI-powered telemedicine platforms expand access to healthcare services, particularly for patients in remote or underserved areas. Virtual consultations and AI diagnostic tools bridge the gap between patients and healthcare providers, improving overall health outcomes.
4. Enhanced Patient Engagement
AI tools such as chatbots and virtual health assistants engage patients more effectively. These tools provide timely information, medication reminders, and personalized health advice, empowering patients to actively manage their health.
Challenges and Considerations
1. Data Privacy and Security
AI in healthcare raises concerns about data privacy and security. Ensuring compliance with regulations and implementing robust cybersecurity measures are essential to protect sensitive patient information and prevent data breaches.
2. Bias and Fairness
AI systems must be trained on diverse and representative datasets to avoid bias. Ensuring that AI tools are fair and equitable is crucial to prevent perpetuating existing health disparities and providing accurate results for all patients.
3. Integration with Existing Systems
Integrating AI with existing healthcare systems can be complex. Compatibility with current workflows and electronic health records (EHRs) must be ensured, and healthcare professionals need proper training to effectively use AI technologies.
4. Ethical and Legal Implications
The use of AI in healthcare raises ethical and legal questions about decision-making and accountability. Clear guidelines and ethical standards are necessary to address these concerns and ensure responsible AI implementation.
The Future of AI in Healthcare
The future of AI in healthcare is promising, with ongoing advancements expected to further enhance patient care. Emerging technologies will likely lead to innovations such as advanced robotic surgeries, real-time health monitoring, and AI-driven wellness plans. Collaboration among healthcare professionals, researchers, and technology developers will be key to unlocking AI’s full potential.
Conclusion
Artificial Intelligence is revolutionizing healthcare by improving diagnostics, personalizing treatments, and enhancing overall patient well-being. While challenges exist, the benefits of AI are substantial, promising a future with more accurate, efficient, and accessible healthcare. As AI technology evolves, its impact on healthcare will continue to grow, driving innovations that enhance the quality of life for patients worldwide.
For more information on how AI is shaping the future of healthcare and its benefits for patient well-being, visit WellBeingProTips.com. For more Visit Our Tiktok, Twitter, and Pinterest.
Understanding Alzheimer’s Disease: Insights, Impacts, and Innovations
Alzheimer’s Disease is a progressive neurological disorder that represents one of the most significant challenges in modern medicine and public health. Characterized by a gradual decline in cognitive function, memory, and behavior, Alzheimer’s Disease affects millions of people globally, with profound implications for individuals, families, and society. This article delves into the nature of Alzheimer’s Disease, its causes and symptoms, its impact on those affected, and the ongoing efforts in research and treatment.
What is Alzheimer’s Disease?
Alzheimer’s Disease is a type of dementia that leads to a continuous decline in cognitive abilities. It is named after Dr. Alois Alzheimer, who first identified the disease in 1906. The disorder primarily affects the brain, leading to the progressive loss of memory, reasoning, and other cognitive functions. Alzheimer’s Disease is the most common form of dementia, accounting for approximately 60-80% of dementia cases.
Causes and Risk Factors
The exact cause of Alzheimer’s Disease remains unknown, but several factors are believed to contribute to its development:
- Genetic Factors:
- Early-Onset Alzheimer’s Disease: This rare form of Alzheimer’s occurs before the age of 65 and is often linked to specific genetic mutations, such as those in the APP, PSEN1, and PSEN2 genes.
- Late-Onset Alzheimer’s Disease: This more common form typically starts after age 65. It is associated with the APOE ε4 allele, a genetic variant that increases the risk of developing the disease.
- Age: Aging is the most significant risk factor. The likelihood of developing Alzheimer’s Disease increases with age, particularly after age 65.
- Family History: Having a first-degree relative with Alzheimer’s Disease increases the risk, suggesting a hereditary component.
- Lifestyle and Health Factors:
- Cardiovascular Health: Conditions such as high blood pressure, diabetes, and high cholesterol may contribute to Alzheimer’s risk.
- Head Trauma: Previous head injuries or concussions may increase susceptibility to Alzheimer’s Disease.
- Education and Cognitive Activity: Lower levels of formal education and reduced cognitive stimulation are associated with an increased risk of Alzheimer’s.
- Environmental and Lifestyle Factors: Emerging research suggests that factors such as diet, physical activity, and exposure to environmental toxins may play a role in the development of Alzheimer’s Disease.
Symptoms and Diagnosis
Alzheimer’s Disease typically manifests through a range of symptoms that worsen over time. These symptoms can be broadly categorized into cognitive and behavioral changes:
- Cognitive Symptoms:
- Memory Loss: Difficulty remembering recent events or conversations is one of the earliest signs of Alzheimer’s Disease.
- Disorientation: Individuals may become confused about time, place, or identity.
- Difficulty with Language: Struggling to find the right words or follow conversations is common.
- Impaired Judgment: Difficulty making decisions or solving problems.
- Behavioral and Psychological Symptoms:
- Mood Swings: Rapid and unpredictable changes in mood can occur.
- Personality Changes: Individuals may exhibit changes in personality, including increased irritability or paranoia.
- Loss of Interest: A decline in interest in activities previously enjoyed.
Diagnosing Alzheimer’s Disease involves a comprehensive assessment that includes:
- Medical History: Reviewing symptoms, family history, and overall health.
- Cognitive Tests: Evaluations to assess memory, problem-solving, and other cognitive functions.
- Neuroimaging: MRI or PET scans to detect brain abnormalities associated with Alzheimer’s Disease.
- Laboratory Tests: Blood tests to rule out other conditions that may cause similar symptoms.
Impact on Individuals and Society
Alzheimer’s Disease has far-reaching effects on individuals and society:
- Personal Impact:
- Declining Independence: As cognitive abilities deteriorate, individuals may struggle with daily activities and personal care, leading to a loss of independence.
- Emotional and Psychological Toll: The progressive nature of the disease can lead to feelings of frustration, depression, and anxiety for both the affected individuals and their caregivers.
- Impact on Families and Caregivers:
- Caregiving Responsibilities: Family members often take on the role of caregivers, which can be physically and emotionally demanding.
- Financial Burden: The costs associated with Alzheimer’s care, including medical expenses and long-term care, can be substantial.
- Societal Impact:
- Economic Costs: Alzheimer’s Disease represents a significant economic burden due to healthcare costs and lost productivity. The costs of care for individuals with Alzheimer’s are expected to rise as the population ages.
- Healthcare Systems: The increasing prevalence of Alzheimer’s Disease places a strain on healthcare systems and resources.
Current Treatments and Research
While there is currently no cure for Alzheimer’s Disease, several treatment options and ongoing research efforts aim to manage symptoms and improve quality of life:
- Medications:
- Cholinesterase Inhibitors: Drugs like donepezil, rivastigmine, and galantamine help improve cognitive function by increasing levels of acetylcholine, a neurotransmitter involved in memory and learning.
- NMDA Receptor Antagonists: Memantine is used to regulate glutamate activity, which can help with symptoms in moderate to severe stages of the disease.
- Non-Pharmacological Interventions:
- Cognitive Therapy: Techniques designed to improve cognitive function and coping strategies.
- Lifestyle Modifications: Encouraging physical activity, social engagement, and a healthy diet to support overall brain health.
- Research and Clinical Trials:
- Biomarker Research: Scientists are investigating biomarkers that can detect Alzheimer’s Disease earlier and track its progression.
- Drug Development: Research is focused on developing new drugs that target the underlying mechanisms of the disease, such as amyloid plaques and tau tangles.
- Gene Therapy and Immunotherapy: Innovative approaches are being explored to modify or suppress the genetic and immune-related factors involved in Alzheimer’s.
Future Directions and Hope
Advances in research and technology offer hope for the future of Alzheimer’s Disease:
- Early Detection: Enhanced diagnostic tools and biomarkers may lead to earlier detection and intervention, potentially slowing disease progression.
- Personalized Medicine: Tailoring treatments to individual genetic profiles and disease characteristics could improve efficacy and outcomes.
- Preventive Strategies: Public health initiatives focusing on lifestyle modifications, cognitive training, and cardiovascular health may help reduce the risk of developing Alzheimer’s.
Conclusion
Alzheimer’s Disease presents one of the most pressing challenges in contemporary healthcare, with its profound impacts on individuals, families, and society. Understanding the causes, symptoms, and effects of the disease is crucial for developing effective management strategies and improving quality of life for those affected. While there is no cure at present, ongoing research and innovative treatments offer hope for better management and, ultimately, a future where Alzheimer’s Disease can be effectively prevented or treated. By advancing our knowledge and investing in research, we can work towards a world where Alzheimer’s Disease no longer represents an overwhelming burden on individuals and society. For more Visit Our Website Tiktok, Twitter, and Pinterest.
Understanding Kidney Disease: Causes, Effects, and Management
Kidney disease is a significant and growing public health concern, impacting millions of individuals worldwide. The kidneys, vital organs in the human body, play crucial roles in filtering blood, removing waste products, balancing electrolytes, and maintaining fluid levels. When these organs become impaired, the consequences can be severe and multifaceted, affecting overall health and quality of life. This article delves into the causes, types, effects, and management of kidney disease, offering insights into how individuals and healthcare systems can address this pervasive issue.
Understanding the Kidneys and Their Functions
The kidneys are two bean-shaped organs located in the lower back, each about the size of a fist. They perform essential functions, including:
- Filtering Blood: The kidneys remove waste products and excess fluids from the bloodstream, which are then excreted as urine.
- Regulating Electrolytes: They help maintain a balance of electrolytes, such as sodium, potassium, and calcium, which are crucial for nerve and muscle function.
- Maintaining Fluid Balance: By adjusting the volume of urine produced, the kidneys regulate the body’s fluid balance.
- Producing Hormones: They produce hormones like erythropoietin, which stimulates red blood cell production, and renin, which helps regulate blood pressure.
Types of Kidney Disease
Kidney disease can manifest in various forms, each with distinct causes and characteristics. The primary types include:
- Chronic Kidney Disease (CKD): Chronic Kidney Disease is a long-term condition where the kidneys gradually lose their ability to function over time. It is often caused by conditions like diabetes, high blood pressure, and glomerulonephritis. CKD is classified into five stages, ranging from mild damage to end-stage renal disease (ESRD), where the kidneys function at less than 15% of their normal capacity.
- Acute Kidney Injury (AKI): Acute Kidney Injury, formerly known as acute renal failure, is a sudden and often reversible loss of kidney function. It can occur due to severe dehydration, infections, toxins, or acute medical conditions. AKI requires prompt medical attention to address the underlying cause and restore kidney function.
- Polycystic Kidney Disease (PKD): Polycystic Kidney Disease is a genetic disorder characterized by the growth of numerous cysts in the kidneys. These cysts can impair kidney function over time and lead to complications such as high blood pressure and kidney stones. PKD can be inherited in an autosomal dominant or recessive pattern.
- Glomerulonephritis: Glomerulonephritis refers to inflammation of the glomeruli, the tiny filtering units within the kidneys. This condition can be caused by infections, autoimmune diseases, or other underlying health issues. It can lead to symptoms such as blood in the urine, swelling, and high blood pressure.
- Kidney Stones: Kidney stones are hard deposits of minerals and salts that form in the kidneys. They can cause severe pain and discomfort as they pass through the urinary tract. Stones may result from factors such as dehydration, high salt intake, or underlying medical conditions.
Causes and Risk Factors
Several factors contribute to the development of kidney disease. Understanding these causes and risk factors is crucial for prevention and early intervention:
- Diabetes: Diabetes is one of the leading causes of chronic kidney disease. High blood sugar levels can damage the blood vessels in the kidneys, impairing their ability to filter waste effectively.
- High Blood Pressure: Chronic hypertension puts extra strain on the kidneys’ blood vessels, leading to damage over time. Managing blood pressure is essential for kidney health.
- Genetic Factors: Genetic predisposition plays a role in certain types of kidney disease, such as polycystic kidney disease and some forms of glomerulonephritis.
- Infections: Severe infections, such as urinary tract infections or sepsis, can impact kidney function if left untreated or if they are recurrent.
- Medication and Toxins: Certain medications and toxins, including over-the-counter pain relievers and illicit drugs, can cause kidney damage when used excessively or improperly.
- Lifestyle Factors: Poor diet, lack of physical activity, and smoking contribute to risk factors like obesity and hypertension, which can adversely affect kidney health.
Symptoms and Diagnosis
Kidney disease may develop gradually, often without noticeable symptoms until it reaches an advanced stage. Common symptoms of kidney disease include:
- Swelling in the legs, ankles, or feet
- Persistent fatigue and weakness
- Changes in urine output or appearance
- High blood pressure
- Pain in the back or sides
Diagnosis involves a combination of medical history, physical examination, and laboratory tests. Key diagnostic tests include:
- Blood Tests: Assess levels of waste products like creatinine and urea, which can indicate kidney function.
- Urine Tests: Detect abnormalities such as protein or blood in the urine.
- Imaging Studies: Ultrasounds, CT scans, or MRIs can visualize kidney structure and detect issues like stones or cysts.
- Kidney Biopsy: In certain cases, a biopsy may be performed to obtain a tissue sample and diagnose specific kidney conditions.
Management and Treatment
Management of kidney disease depends on the type and stage of the condition. The goals are to slow progression, manage symptoms, and prevent complications. Key approaches include:
- Lifestyle Modifications:
- Dietary Changes: Reducing sodium, protein, and potassium intake can help manage kidney disease. A renal dietitian can provide personalized recommendations.
- Exercise: Regular physical activity helps control blood pressure, blood sugar levels, and weight.
- Smoking Cessation: Quitting smoking improves overall health and reduces kidney disease risk.
- Medications:
- Blood Pressure Medications: ACE inhibitors or angiotensin receptor blockers can help manage hypertension and protect kidney function.
- Diuretics: These help reduce fluid buildup and manage symptoms like swelling.
- Medications for Diabetes: Controlling blood sugar levels is crucial for those with diabetes-related kidney disease.
- Dialysis: In advanced stages of kidney disease, when the kidneys can no longer filter blood effectively, dialysis may be required. There are two main types:
- Hemodialysis: Blood is filtered through a machine outside the body.
- Peritoneal Dialysis: A special fluid is introduced into the abdominal cavity to filter waste from the blood.
- Kidney Transplant: For end-stage renal disease, a kidney transplant may be the best option. A healthy kidney from a donor is surgically implanted to replace the damaged kidneys.
Prevention and Public Health Strategies
Preventing kidney disease involves addressing risk factors and promoting early detection. Public health strategies include:
- Education and Awareness: Raising awareness about kidney health, risk factors, and symptoms can lead to early diagnosis and better management.
- Screening Programs: Regular screening for high-risk individuals, such as those with diabetes or hypertension, helps catch kidney disease early.
- Access to Healthcare: Ensuring access to affordable healthcare and medications supports the management of chronic conditions that can lead to kidney disease.
Conclusion
Kidney disease is a multifaceted health issue with significant implications for individuals and healthcare systems. Understanding the types, causes, symptoms, and management strategies is essential for prevention and effective treatment. By addressing risk factors, promoting healthy lifestyles, and supporting early detection and intervention, we can improve kidney health and overall well-being. Collaboration among individuals, healthcare providers, and public health initiatives is key to combating this prevalent and impactful condition. For more Visit Our Website Tiktok, Twitter, and Pinterest.
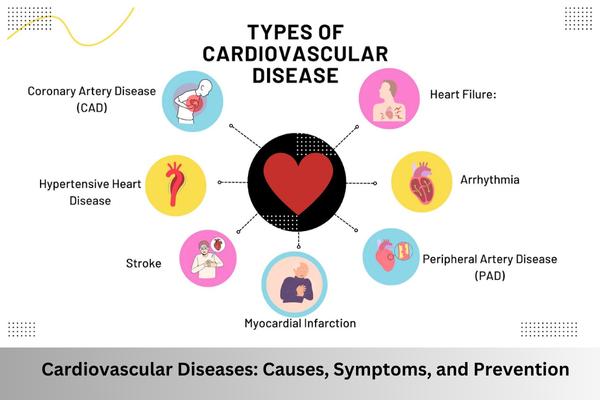
Understanding Cardiovascular Diseases: Causes, Symptoms, and Prevention
Cardiovascular diseases (CVDs) are a leading cause of death worldwide, affecting the heart and blood vessels. This comprehensive guide explores the various types of cardiovascular diseases, their causes, symptoms, and preventive measures. By understanding these aspects, you can take proactive steps to maintain heart health and reduce your risk of these serious conditions.
What Are Cardiovascular Diseases?
Cardiovascular diseases include a range of conditions affecting the heart and blood vessels. Common types of CVDs are:
- Coronary Artery Disease (CAD): This condition arises when the coronary arteries become narrowed or blocked due to plaque buildup. CAD can lead to chest pain (angina) and heart attacks.
- Heart Attack (Myocardial Infarction): A heart attack occurs when blood flow to a portion of the heart muscle is blocked for an extended period, resulting in damage to the heart tissue.
- Stroke: Strokes happen when blood flow to a part of the brain is disrupted, either due to a blockage (ischemic stroke) or bleeding (hemorrhagic stroke), causing brain damage.
- Hypertension (High Blood Pressure): Hypertension involves consistently elevated blood pressure levels, which can damage arteries and lead to heart disease, stroke, and kidney issues.
- Heart Failure: Known as congestive heart failure, this condition occurs when the heart cannot pump blood effectively, leading to fluid buildup in the lungs and other areas.
- Peripheral Artery Disease (PAD): PAD involves the narrowing of peripheral arteries, usually in the legs, which can cause pain and cramping during physical activity.
Causes and Risk Factors
Cardiovascular diseases are influenced by various risk factors. These can be categorized into modifiable and non-modifiable factors:
Non-Modifiable Risk Factors
- Age: The risk of cardiovascular diseases increases with age. Men generally face a higher risk earlier than women.
- Gender: Men are typically at higher risk for cardiovascular diseases at a younger age. Women’s risk increases and may surpass that of men after menopause.
- Family History: A family history of cardiovascular diseases can elevate your risk, suggesting a genetic predisposition.
- Genetics: Genetic mutations and inherited conditions can increase the likelihood of developing cardiovascular diseases.
Modifiable Risk Factors
- Smoking: Tobacco use is a major risk factor, damaging blood vessels, promoting plaque buildup, and reducing oxygen supply to the heart.
- Diet: Diets high in saturated fats, trans fats, cholesterol, and sodium can lead to cardiovascular diseases. Consuming a diet rich in fruits, vegetables, whole grains, and lean proteins is crucial for heart health.
- Physical Inactivity: Lack of regular exercise can lead to obesity, high blood pressure, and elevated cholesterol levels, increasing cardiovascular disease risk.
- Obesity: Excess weight, especially abdominal fat, is associated with higher risks of hypertension, diabetes, and heart disease.
- Excessive Alcohol Consumption: Drinking alcohol in excess can raise blood pressure, contribute to obesity, and increase cardiovascular disease risk.
- Stress: Chronic stress may lead to unhealthy behaviors such as smoking or overeating and negatively affect heart health.
- High Blood Pressure: Persistent high blood pressure puts extra strain on the heart and blood vessels, increasing the risk of heart disease and stroke.
- High Cholesterol Levels: Elevated levels of low-density lipoprotein (LDL) cholesterol and low levels of high-density lipoprotein (HDL) cholesterol contribute to arterial plaque buildup.
Symptoms of Cardiovascular Diseases
Recognizing the symptoms of cardiovascular diseases is crucial for early detection and treatment. Common symptoms include:
- Chest Pain or Discomfort: Often described as pressure, squeezing, or aching in the chest, which can signal coronary artery disease or a heart attack.
- Shortness of Breath: Difficulty breathing, especially during physical activity, may indicate heart failure or other heart conditions.
- Palpitations: Irregular or rapid heartbeats can be a sign of arrhythmias or other heart issues.
- Fatigue: Unusual tiredness or weakness, especially with physical exertion, can point to heart failure or cardiovascular problems.
- Swelling: Fluid buildup in the legs, ankles, or abdomen can be associated with heart failure.
- Dizziness or Lightheadedness: Feeling faint or unsteady may be related to heart conditions or a drop in blood pressure.
- Pain or Numbness in Limbs: Pain, numbness, or cramping in the legs, particularly during exercise, can indicate peripheral artery disease.
Prevention and Management
Preventing and managing cardiovascular diseases involves lifestyle changes and regular health monitoring:
- Healthy Diet: Eat a balanced diet rich in fruits, vegetables, whole grains, and lean proteins. Limit intake of saturated fats, trans fats, cholesterol, and sodium.
- Regular Exercise: Engage in at least 150 minutes of moderate-intensity exercise per week, such as brisk walking or cycling, to maintain a healthy weight and improve cardiovascular health.
- Smoking Cessation: Quit smoking and avoid exposure to secondhand smoke. Seek support if needed to help with smoking cessation.
- Moderate Alcohol Consumption: If you drink alcohol, do so in moderation—up to one drink per day for women and two drinks per day for men.
- Manage Stress: Practice stress management techniques like mindfulness, meditation, or hobbies to reduce stress levels and improve heart health.
- Regular Check-Ups: Monitor your blood pressure, cholesterol levels, and overall heart health with regular medical check-ups. Follow your healthcare provider’s advice for managing any conditions.
- Medication Adherence: If prescribed medication for high blood pressure, cholesterol, or other cardiovascular issues, take it as directed by your healthcare provider.
Conclusion
Cardiovascular diseases are a significant health issue globally, but many risk factors can be managed or prevented through lifestyle changes. By understanding the causes, recognizing symptoms, and adopting preventive measures, you can take proactive steps to protect your heart health. Regular check-ups, a heart-healthy diet, regular exercise, and avoiding harmful behaviors are essential for maintaining cardiovascular well-being.
Early detection and management of risk factors can greatly reduce the impact of cardiovascular diseases, leading to a healthier and longer life. Prioritizing heart health through informed choices and proactive measures is key to reducing the prevalence and severity of cardiovascular diseases. For more Visit Our Website Tiktok, Twitter, and Pinterest.
Understanding Tick-Borne Diseases: Risks, Symptoms, and Prevention
Ticks are not just an outdoor nuisance; they are vectors for several serious diseases that can affect both humans and animals. With increasing global temperatures and expanding human activities, the incidence of tick-borne diseases is rising. This comprehensive guide explores tick-borne diseases, including their symptoms, prevention strategies, and their impact on public health.
What Are Tick-Borne Diseases?
Tick-borne diseases are illnesses transmitted through the bite of an infected tick. Ticks are small arachnids that feed on the blood of their hosts and can carry various pathogens such as bacteria, viruses, and protozoa. When a tick feeds on an infected host, it can pass these pathogens to other hosts during subsequent feedings.
Common Tick-Borne Diseases
- Lyme Disease
- Caused By: Borrelia burgdorferi, a type of bacteria.
- Symptoms: Look out for symptoms like fever, headache, fatigue, and a distinctive “bull’s-eye” rash known as erythema migrans. If untreated, it may progress to joint pain, neurological issues, and heart problems.
- Treatment: Antibiotics, such as doxycycline, are effective, especially when administered early.
- Rocky Mountain Spotted Fever (RMSF)
- Caused By: Rickettsia rickettsii, a type of bacteria.
- Symptoms: High fever, rash, headache, and muscle aches. The rash often starts at the wrists and ankles and spreads to the trunk.
- Treatment: Doxycycline is the standard treatment. Early intervention is crucial to prevent severe complications.
- Anaplasmosis
- Caused By: Anaplasma phagocytophilum, a type of bacteria.
- Symptoms: Fever, headache, muscle aches, nausea, and vomiting are common. Symptoms often resemble flu-like conditions.
- Treatment: Managed with doxycycline. Early diagnosis is important for effective treatment.
- Babesiosis
- Caused By: Babesia microti, a protozoan parasite.
- Symptoms: High fever, chills, and sweating, similar to malaria. Severe cases can lead to complications, especially in those with weakened immune systems.
- Treatment: Combination of antiparasitic medications and antibiotics. Severe cases may require hospitalization.
- Ehrlichiosis
- Caused By: Ehrlichia chaffeensis, a type of bacteria.
- Symptoms: Fever, headache, fatigue, and muscle aches are common. It can be challenging to diagnose due to symptom overlap with other tick-borne diseases.
- Treatment: Typically treated with doxycycline. Early treatment helps prevent severe outcomes.
- Tick-Borne Encephalitis (TBE)
- Caused By: Tick-borne encephalitis virus.
- Symptoms: Initial symptoms include fever, headache, and muscle pain, which may progress to neurological issues like confusion and paralysis.
- Treatment: No specific antiviral treatment exists. Supportive care and symptomatic management are key. Vaccination is available in some regions.
Diagnosing Tick-Borne Diseases
Diagnosing tick-borne diseases can be challenging due to symptom overlap with other illnesses. Diagnostic approaches typically involve:
- Clinical Evaluation: Assessment based on symptoms and recent tick exposure.
- Laboratory Tests: Blood tests to detect antibodies or pathogens. Some diseases have specific tests, but false negatives are possible.
Prevention Strategies for Tick-Borne Diseases
- Personal Protection
- Use Insect Repellent: Apply repellents containing DEET, picaridin, or oil of lemon eucalyptus to exposed skin and clothing.
- Wear Protective Clothing: When outdoors, wear long sleeves, long pants, and tuck pants into socks.
- Tick Checks: Conduct regular tick checks after outdoor activities. Remove ticks promptly using fine-tipped tweezers.
- Environmental Management
- Maintain Landscaping: Keep grass mowed and remove leaf litter and tall vegetation around homes to reduce tick habitat.
- Create Barriers: Use landscaping to establish tick-free zones between wooded areas and recreational spaces.
- Awareness and Education
- Know Your Risks: Be aware of tick activity in your area, which can be seasonal and vary by geography.
- Educate Others: Share information about tick-borne diseases and prevention strategies within communities and among outdoor enthusiasts.
Climate Change and Tick-Borne Diseases
Climate change is influencing tick populations and the spread of tick-borne diseases. Warmer temperatures and changing precipitation patterns can expand tick habitats into new regions, increasing the risk of tick-borne diseases. Staying informed and adapting prevention strategies are crucial in light of these changes.
Public Health Response to Tick-Borne Diseases
Public health agencies are essential in managing tick-borne diseases through:
- Surveillance: Monitoring tick populations and disease incidence to identify emerging threats.
- Research: Funding research to develop new treatments, vaccines, and diagnostic tools.
- Public Education: Providing information on prevention and treatment to the public.
Conclusion
Tick-borne diseases represent a significant health risk that requires awareness, prevention, and timely treatment. With increasing tick populations and shifting climate patterns, understanding and managing these diseases is crucial. By adopting preventive measures, conducting regular tick checks, and seeking prompt medical care, individuals can reduce their risk of tick-borne illnesses. Public health efforts and ongoing research will continue to play a vital role in addressing these diseases and protecting public health. For more Visit Our Website Tiktok, Twitter, and Pinterest.